High blood pressure (hypertension) is common
High blood pressure is well recognised to be very common in middle age and elderly population. It is a major risk factor in adverse cardiovascular outcomes including stroke, coronary artery disease, aortic aneurysm and other vascular disease [1, 2]. The real challenge with high blood pressure is that it is almost always silent and causes no symptom – you may feel completely well and normal. Often patients are unaware of their silent high blood pressure until it causes damage to the kidneys, brain, heart muscle, or worse still, presents with an acute stroke or heart attack.
We have discussed how we investigate known hypertensive patients in terms of biochemical tests, as well as cardiac, and vascular imaging. However, what is the evidence to suggest we should actively look out or screen for hypertension in younger adults and does undetected raised blood pressure really contribute to higher risks of cardiovascular events in later life?
Why is early preventive cardiology important?
A recent study by a Chinese group published in the British Medical Journal [3] sought to evaluate and quantify the future risk of cardiovascular events in young adults with sub-optimally managed high blood pressure.
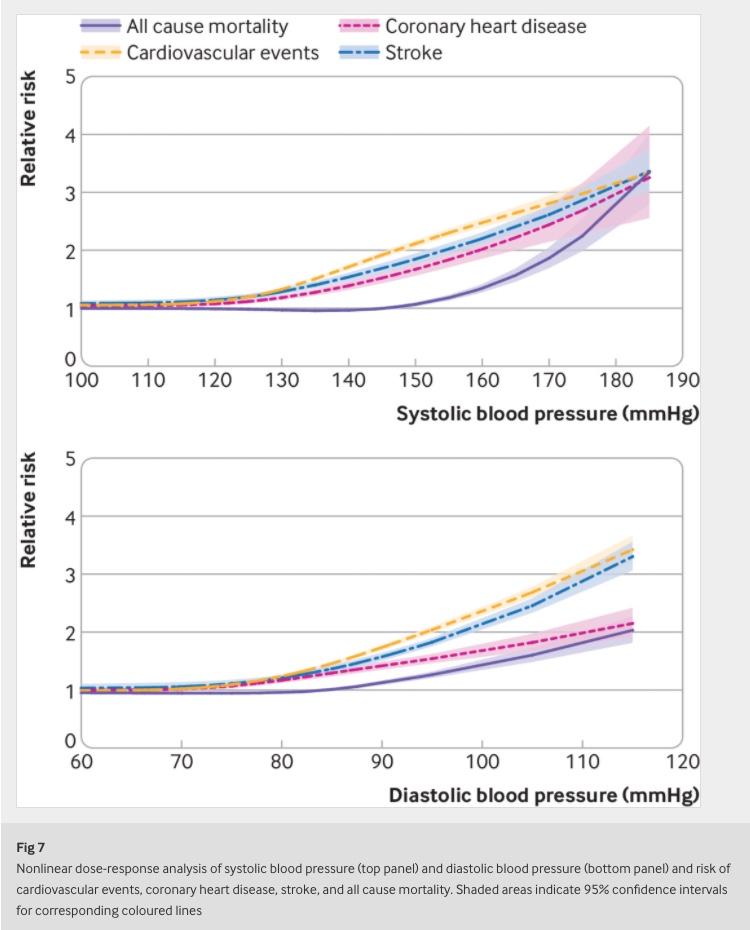
The authors performed a meta-analysis of 17 observational studies involving 4.5 million young adults between 18-45 years with high blood pressure with a mean follow-up period of 14.7 years. It showed that both systolic (top number) and diastolic (bottom number) blood pressure are independently associated with an increased risk of future adverse cardiovascular events (e.g. stroke, coronary artery disease, death).
The progressive association between blood pressure and adverse cardiovascular events is striking:
The implication of this association suggests that even for moderate degree of raised blood pressure in younger adults e.g. systolic blood pressure 150mmHg and diastolic blood pressure 95mmHg, if left undetected and untreated, can increase the risk of future stroke and heart attack by two-fold compared to individuals with a “standard” normal blood pressure 120/70mmHg. This is literally doubling the risk!
Specialist private care by the expert cardiologists at CardioQinetics
It is, therefore, well worth to be vigilant about silent high blood pressure. At-risk individuals (e.g. those with a family history of high blood pressure, a family history of premature cardiovascular disease, and those suffering from diabetes mellitus, etc.) in Buckinghamshire, Berkshire, or West London should seek expert help with our trusted specialist cardiologist. We can evaluate and monitor your blood pressure with ambulatory automatic blood pressure diary and offer effective pharmacological, as well as non-pharmacological intervention to reduce your future cardiovascular risk and prevent serious health problem in the future.
In addition, our cardiologists may also recommend one or more potential investigative tests such as:-
- Echocardiography to quantify heart muscle and valve function
- Cardiac / aortic CT to look for dilatation or restriction of blood vessels
- Ultrasound scan of the kidneys
- Blood or urine tests to screen for causes of secondary hypertension, if indicated.
Reference:
- Han M, Li Q, Liu L, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens2019;37:2325-32. doi:10.1097/HJH.0000000000002191. pmid:31335511
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet2018;392:1736-88. doi:10.1016/S0140-6736(18)32203-7. pmid:30496103
- Luo D, Cheng Y, Zhang H, et al. Association between high blood pressure and long term cardiovascular events in young adults: systematic review and meta-analysis. BMJ 2020;370:m3222 (DOI: dx.doi.org/10.1136/bmj.3222)