As an interventional cardiologist, I often get asked by patients (and friends and family as well no doubt!) regarding my view on statins.
Statin therapy remains the most important corner stone of modern cardiovascular risk management. In recent years, however, there is a minority view gaining traction in the alternative medicine / niche conspiracy theory / social media sphere, with many portraying statins (as well as many other drugs) as part of a large conspiracy by the "Big Pharma" to lock us into a lifetime of tablets for the maximal corporate greed. Lest not forget that most statins are now off-patent and available as generic drugs - so a month's supply of one of the commonest used statin Atorvastatin at 40mg now costs less than £2.00 / month and the money goes to smaller independent pharmaceutical companies making generic drugs anyway, rather than the "Big Pharma" per se.
In this 3 parts blog series, I will explore the fallacy of some alleged claims against statins, a brief overview of the vast amount of data available to guide informed decisions on statin therapy, as well as some latest research on how statin stacked up against other traditional (or no!) therapy in China. I will also look at how "statins causing muscle ache" was elegantly debunked. Finally, I will discuss how we calculate cardiovascular risk and decide who will benefit from statin therapy, as well as how we should utilise non-invasive imaging tools to achieve individual personalised medicine in 21st century.
Drug therapy versus non-pharmacological intervention
Preventive cardiology aims to reduce cardiovascular mortality and morbidity through a combination of education, non-pharmacological intervention [NPI] (such as diet, exercise, general well-bring or even sleep intervention!), as well as judicious use of evidence-based pharmacological intervention i.e. drugs.
In the strange cyber-world we live in today, particularly with the heavy influence of unregulated social media and tabloid news outlets, some individuals unfortunately form a rather extreme radical view on NPI or other “natural” or “herbal” therapy versus established drug therapy – often with devastating consequences.
First of all, let’s be very clear with 3 facts upfront:–
- The vast majority of currently available drugs are derivatives of naturally occurring biological molecules or synthetic compounds that mimic the function of such;
- There is no meaningful difference – either biologically or semantically – between derivatives of naturally occurring biological molecules (often from plants) and your natural “herbal” therapy;
- Any molecule or substance that are potent enough to alter biological states (treating diseases) will inevitably cause some undesirable effects (side-effects) in some individuals – otherwise it is simply either biologically inert or used in concentration way too low to exert any effect – it is then simply homeopathy!
And if you believe in homeopathy, no offence, but you should probably stop reading my article right now :-)
There are many examples of the unnecessary artificial conflict between evidence-based pharmacological intervention i.e. drugs versus natural (often herbal) therapy in a range of human conditions or diseases. In cardiovascular medicine, we see this artificial conflict most vividly in the combat against high blood pressure (hypertension), diabetes, and most particularly and in high profile cases against high cholesterol (dyslipidaemia). People from certain cultural backgrounds may be more prone to this artificial, almost ideological, conflict. For example, China and many South-East Asian countries have a long history of traditional herbal medicine. I am not in any way diminishing its value or importance and some of these herbal therapy might very well exert positive biological effects – but let’s not forget the 3 upfront facts recalled above – these biological compounds in traditional herbal medicine are no different to drug therapy and if they are potent enough to treat human diseases, they will likely cause side-effects too!
Slightly off-tangent here but nonetheless an interesting point - traditional Chinese medicine (TCM) has a long distinguished history; and although using very different principles compared to modern western medicine, it has no doubt been effective in combating many human diseases in ancient China / Asia. Historically, however, the biggest natural killers in ancient time were trauma and infectious diseases and the average men/women rarely live past their 50s-60s. A lot of modern diseases such as diabetes (type 2), atherosclerotic diseases such as heart attacks and strokes, and even cancers are diseases of older age, often linked with modern affluent sedentary lifestyles. These disease entities did not really exist, or caused any significant health burden, in ancient societies. In my view, therefore, this is unfair and we should never expect TCM to be effective in tackling modern diseases in cardiovascular medicine.
Statins and cardiovascular risk reduction
Coming back to preventive cardiology and cardiovascular risk reduction. HMG-CoA reductase inhibitors (statins) have been the corner stone in combating premature cardiovascular mortality and morbidity since the first definitive trial in 1994 [1] showing reduction in death and future heart attack in patients with known coronary artery disease. In the ensuing three decades, numerous randomised controlled trials have confirmed the irrefutable beneficial effects of statin – both in primary prevention (to prevent cardiovascular disease in healthy people) and in secondary prevention (prevent further disease in people with existing cardiovascular conditions).
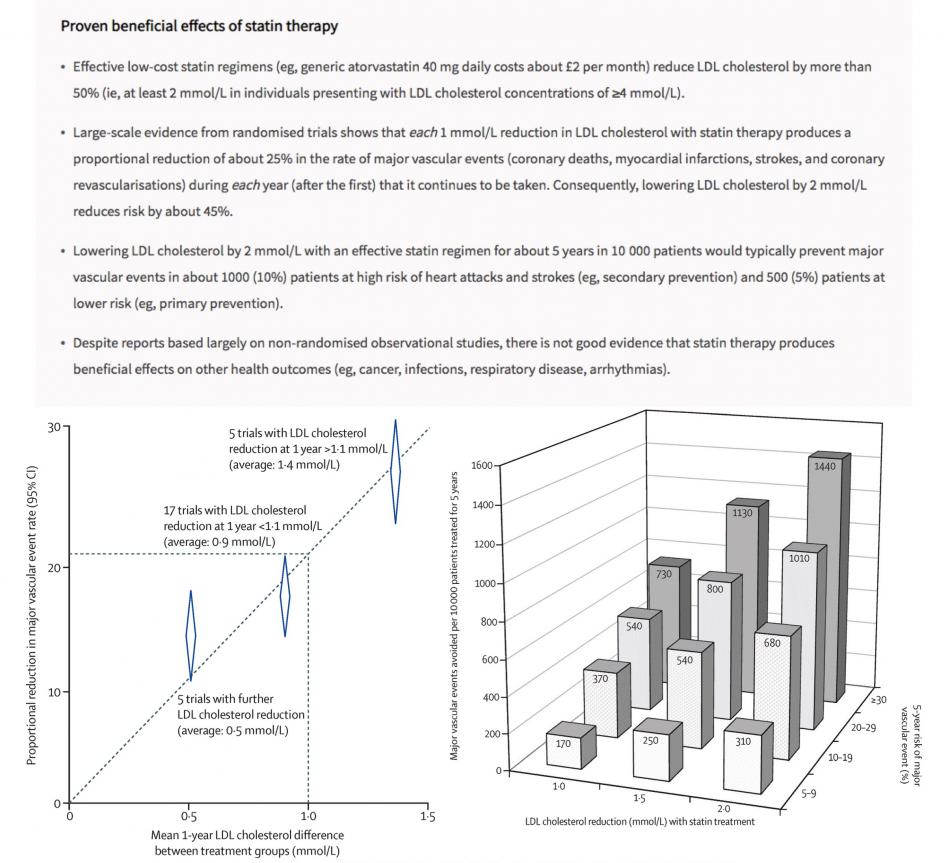
The concept of primary prevention in preventive cardiology can sometimes be difficult and challenging to communicate to patients. Given that statins, just like many other natural “herbal” medicines, do have some recognised but infrequent adverse effects. Typically, treatment of 10,000 patients for 5 years with an effective regimen (eg, atorvastatin 40 mg daily) would cause about 5 cases of myopathy (one of which might progress, if the statin therapy is not stopped, to the more severe condition of rhabdomyolysis), 50–100 new cases of diabetes, and 5–10 haemorrhagic strokes.[2] Overall, however, large-scale evidence from randomised trials shows that statin therapy reduces the risk of major cardiovascular events (e.g. heart attacks, strokes, need of coronary stenting, or cardiac death) by 25% for each mmol/L reduction of LDL-c during each year that it continues to be taken – and that any adverse impact of the side-effects on major vascular events has already been taken into account in the estimates of the absolute benefits.[2]
Detailed exploration of the vast amount of data from numerous statin trials is beyond the scope of this mini blog series; but for those interested, Professor Sir Rory Collins in Oxford has penned a very comprehensive and authoritative review to help clinicians, patients, and the public to make informed decisions about statin therapy – click here to read more. (https://doi.org/10.1016/S0140-6736(16)31357-5)
In Part 2 of the blog series, we will continue our journey to explore some latest research on how statin stacked up against other traditional (or no!) therapy in China. We will also look at how "statins causing muscle ache" was recently debunked once more. Stay tuned :-)
Reference
- The Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383-9
- Collins R, Reith C, Emberson J, Armitage J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016;388(10059):2532-61 [doi.org/10.1016/S0140-6736(16)31357-5]
- Jia Y, Wen J, Qureshi R, et al. Effect of redundant clinical trials from mainland China evaluating statins in patients with coronary artery disease: cross sectional study. BMJ 2021;372:n48 [doi.org/10.1136/bmj.n48]
- Herrett E, Williamson E, Brack K, et al. Statin treatment and muscle symptoms: series of randomised, placebe controlled n-of-1 trials. BMJ 2021;372:n135 [doi.org/10.1136/bmj.n135]
- Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 2020;41(1):111-88.